In the last 3 posts, I have covered the common cold (rhinovirus), its underlying mechanisms of action, the immunological benefits of vitamin C/quercetin/zinc, and how they inhibit and control viral entry, replication, and inflammatory cascades. In the following sections, I will be considering vitamin D3 as another viable means of supporting the immune system.
D3, also known as cholecalciferol, has become widely known for its ability to correct rickets; a childhood disease characterized by sub-optimal bone development.1 D3 is fairly rare in the diet, but can be found in fatty fish (i.e., sardines, tuna, salmon, swordfish) and to a lesser extent in shitake mushrooms, butter, cheese, eggs, yogurt, and milk.1(389) D3 is known to play complex roles within the body and supports bone homeostasis (most widely recognized) as well as cell differentiation, proliferation/growth, muscle structure and function.1(393) Please see below links for other benefits of D3 that I have written about previously:
Vitamin D: Types, Utility, Screening, and Optimal Dosing
Determining Optimal Vitamin D3 Levels
Vitamin D3 and Crohn’s Disease
Vitamin D and Essential Hypertension
Vitamin D3 and Prostate Cancer
Multiple Sclerosis and Vitamin D3
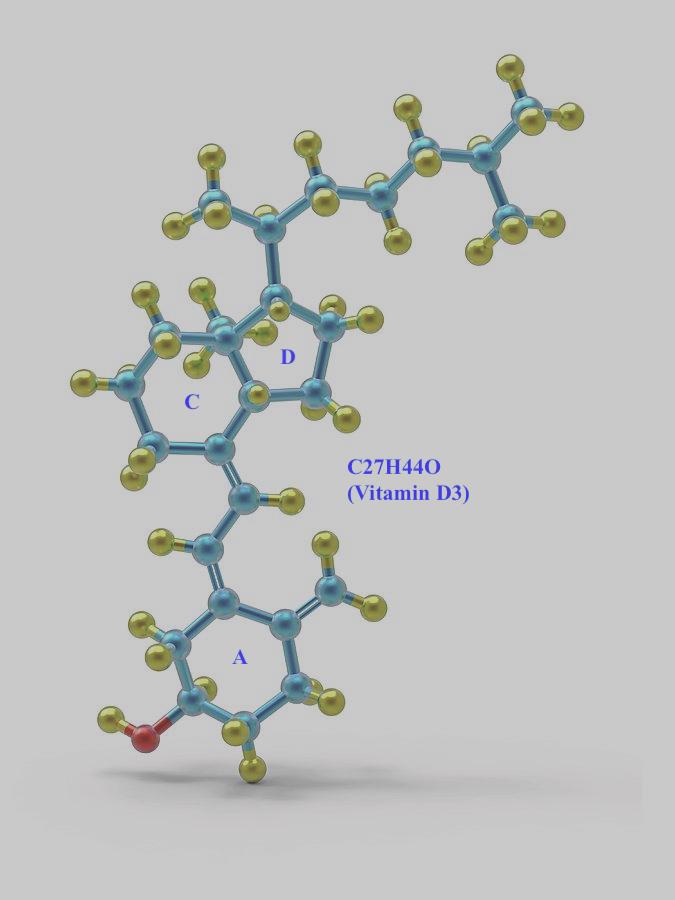
D3 is a particularly unique substance because of its structure; D3 is a pre-hormone since it contains 3 ring structures (A, C, D).1(389) Once D3 has OH (hydroxyl groups) added to its structure with the help of the liver and kidneys, it becomes 1,25-(OH2)D.2 Most relevantly, 1,25-(OH2)D is considered the biologically active form of D3, making it a hormone; any substance that controls and regulates the activity of target cells and organs.3
Notice (pic below) D3 has 1 OH, but 1,25-(OH2)D has 2 other OH groups added
Interestingly, and unknown to most individuals, D3 interacts with an excess of 200 genes, meaning that D3 directly affects gene expression; the process by which proteins and structures are made in the body.1(392) Furthermore, D3 receptors (parts of a cell that interacts with D3) are found in over 30 organs to include the skin, muscle, kidneys, intestine, bone, and lungs.1(393) Of particular interest, and focus of this article, will be D3’s modulatory effects upon the common cold and its downstream effects upon the lungs.
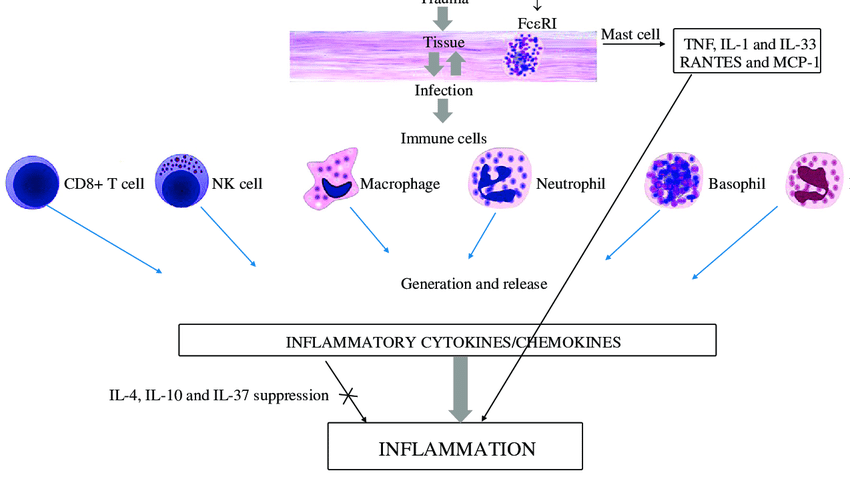
As mentioned in previous articles, viruses tend to induce a cellular environment favorable for their need to replicate. Part of this change can include an increase in a cellular oxidation and an increased inflammatory state by manipulating the cell/immune system. The immune system requires a degree of inflammation to carry out its tasks. Specifically, an optimal level of inflammation is ideal; not too much, not too little. For example, an excessive innate/adaptive immune response is once that characterizes many autoimmune diseases; a process where the immune system attacks the cells and tissues of one’s own body. Such would exemplify an overactive/uncontrolled response of the immune system.
D3 is found amongst several constituents of the immune system to include activated T cells (adaptive immune system) and monocytes/dendritic cells (innate immune system).4 Interestingly, in-vitro (cell studies) indicated that D3 inhibited pro-inflammatory activity of CD4+ (aka T-helper cells of the adaptive immune system) by down-regulating interleukin 2 (IL-2) and tumor necrosis factor alpha (TNF-α); IL-2 stimulates activity of natural killer cells while TNF-α stimulates cell death.5
D3 has also been shown to specifically stimulate T helper cells 2 (TH2) and down-regulate T helper cells 1 (TH1) responses by optimizing interleukin-4 (IL-4), interleukin-5 (IL-5), and interleukin-10 (IL-10) production.4(4) Such is relevant because TH2 cells help control antibody-mediated immune responses, producing a more anti-inflammatory state in cells and tissues, while TH1 activity drives inflammatory responses.4(4) Dendritic cells (DCs) and macrophages also appear to respond to the presence of D3; initially, D3 stimulates their maturation/function (DCs, and macrophages to a lesser extent, present antigens to the adaptive immune system) yet the receptors on the DC/macrophages that “speak” with D3 decrease in number inhibiting further maturation of DCs/macrophages. Such may occur so that an overzealous response of DC/macrophage antigen presentation, and inflammation, is limited.4(5)
In conclusion, I have covered the common cold (rhinovirus), its underlying mechanisms of action, the immunological benefits of vitamin C/quercetin/zinc, D3, and how they inhibit and control viral entry, replication, and inflammatory cascades. As an aggregate, I believe that these 4 supplements can work in a complementary fashion to help support the immune system. When used judiciously, such supplements should help support health, performance, and longevity.
References
1. Gropper SS, Smith JL, Carr, TP. Advanced Nutrition and Human Metabolism. 7th ed. Boston, MA: Cengage Learning; 2018.
2. Lord RS, Bralley JA. Laboratory Evaluations for Integrative and Functional Medicine. 2nded. Duluth, GA: Genova Diagnostics; 2012.
3. Kenney WL, Wilmore JH, Costill DL. Physiology of Sport and Exercise. 5th ed. Champaign, IL: Human Kinetics; 2012.
4. Yang CY, Leung PSC, Adamopoulos IE, et al. The implication of vitamin D and autoimmunity: a comprehensive review. Clin Rev Allergy Immunol. 2013;45(2):217-226. doi: 10.1007/s12016-013-8361-3.
5. Idriss HT, Naismith JH. TNF alpha and the TNF receptor superfamily: structure-function relationships. Micros Res Tech. 2000; 50(3): 184-195. doi:10.1002/1097-0029(20000801)50:3<184::AID-JEMT2>3.0.CO;2-H.
-Michael McIsaac